The partnership aspires to advance the knowledge of transformational change for educators, technical experts and researchers, as well as practitioners.
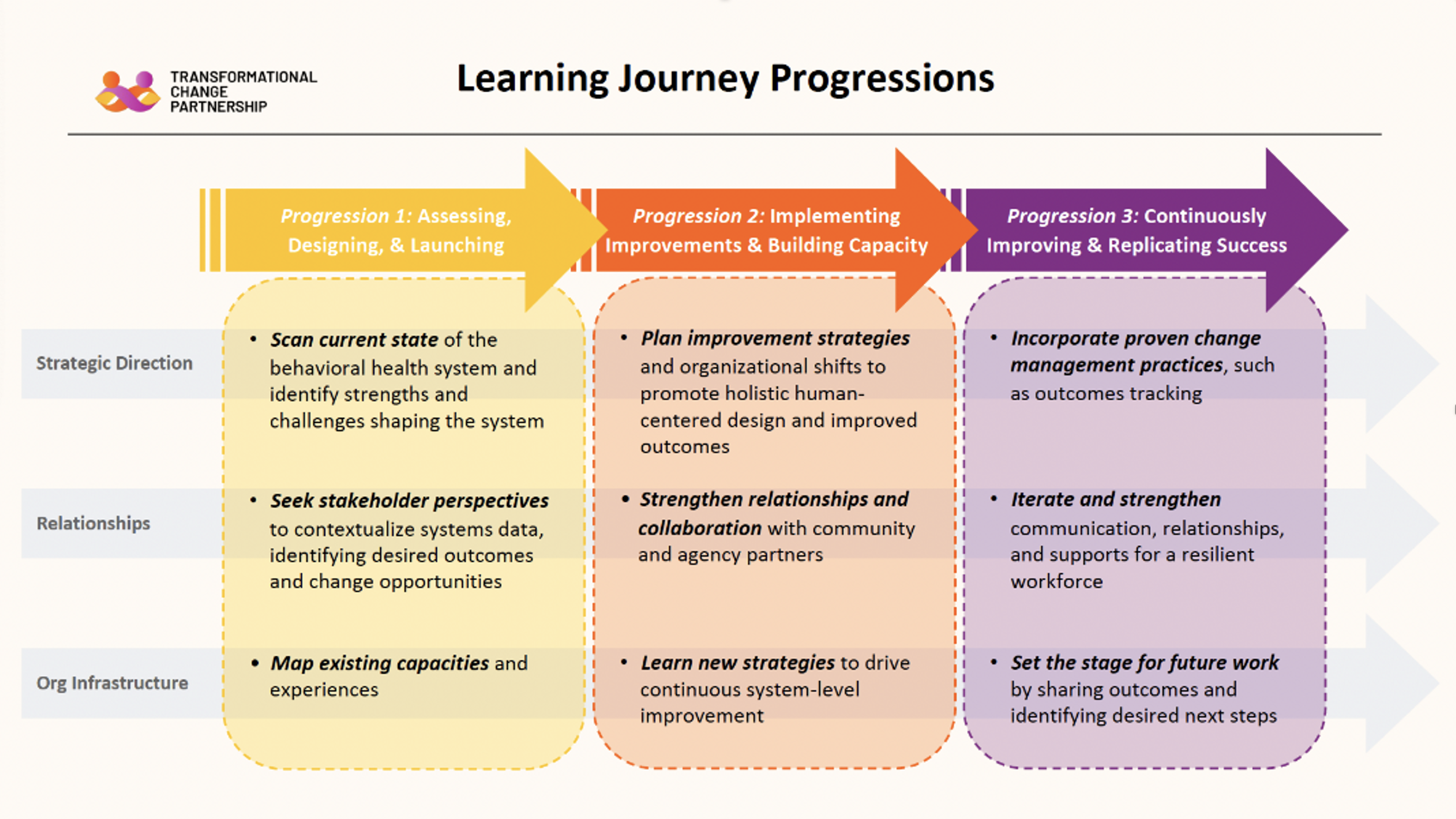
In designing the program, the partners developed a conceptual learning model that articulated what participants need to know, need to know how to do, need to experience and need to feel.
Based on that assessment, a set of “change building blocks” were developed that incorporated that necessary knowledge, skills and abilities. Progressions were developed to align and integrate the information for participants from the building blocks into the process of designing and implementing an improvement project.
The Partnership is assembling and synthesizing the research base for each of the change building blocks, as well as analysis and experience from implementation and replication efforts.
None of the change building blocks are new to the field of system change, and some of them are tested and reliable elements of change management. However, some of the elements are relatively new, rapidly maturing and have only recently been applied to behavioral health or broader efforts to improve the social determinants of health.
For example, community engagement strategies are rapidly maturing beyond providing information or even consulting with the public to empowering community members to set priorities and shape the design of services. Those developing practices are being integrated with human-centered design to rethink all aspects of service delivery, with the additional intent of tailoring services to racial and cultural characteristics of communities and individuals to reduce disparities in access, quality and outcomes.
Work products developed through this activity will be posted to inform discussions, discernment and ongoing improvements to the Partnership and the field of transformational change.