Breadcrumb
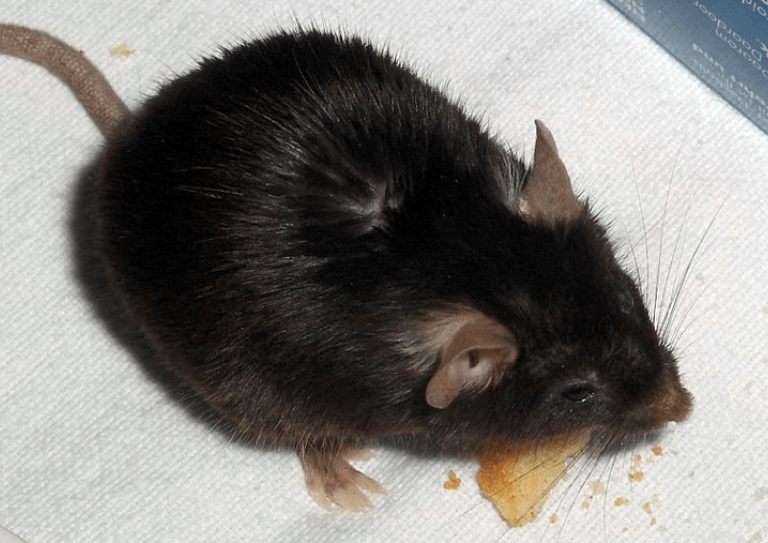
Mouse Model Demonstrates Strain Differences in Susceptibility to Opioid Side Effects
What is it?
Research on mice to determine if genetics influence the responses to and side effects from opioids — in particular, constipation and depressed breathing.
What problem does it aim to solve?
Opioids are an invaluable form of pain relief, but their side effects can be difficult to tolerate, and can even be life threatening. Determining what factors make it more likely that side effects will occur could help shape treatment recommendations for individuals as well as future drug development.
How does it work?
Researchers took 20 mice from two different genetic backgrounds, A/J and C57BL/6J, and randomly divided them into 4 groups. In the first experiment, the members of each group were injected with either 5 mg/kg or 40 mg/kg of morphine, then monitored to see how their breathing slowed and their air intake decreased. In the second experiment, all the mice were injected three times a day with either saline or morphine at doses of 5, 15, 40 or 60 milligrams per kilogram of body weight (mg/kg) and then given charcoal slurry to measure how the passage of material through the intestines slows down under the influence of opioids.
What are the real-world implications?
The A/J strain of mice responded differently than the C57BL/6J mice. In particular, the C57BL/6J demonstrated stronger responses to opioids; their breathing decreased and the passage of charcoal through their intestines slowed more than was the case for the A/J mice. Because all mice were raised and treated the same way, the differences are caused by genetics rather than environmental causes.
What are the next steps?
More studies should be performed to determine what specific genes are responsible for the difference in side effects. This can help both to determine what opioids are best for a given individual and to develop new classes of opioids with fewer side effects.

The C57BL/6J strain of mice responds more strongly to opioids.
Source
“Mouse model demonstrates strain differences in susceptibility to opioid side effects”, Neuroscience Letters, Volume 675, 14 May 2018, Pages 110-115
Authors
Andrew Young, Department of Diagnostic Sciences, Arthur A. Dugoni School of Dentistry
Archana Viswanath, Department of Oral and Maxillofacial Surgery, Tufts University School of Dental Medicine
Mythili Kalladka, Eastman Institute for Oral Health
Junad Khan, Eastman Institute for Oral Health
Eli Eliav, Eastman Institute for Oral Health
Scott R. Diehl, Department of Oral Biology, Rutgers School of Dental Medicine